Based on the searches conducted in the investigated databases, 836 articles were extracted, respectively after removing duplicates n = 495, dissertation between the title of the article with the research topic n = 132 and lack of connection between the abstract and the aims of the present study n = 102, 108 articles remained. (Fig. 1).
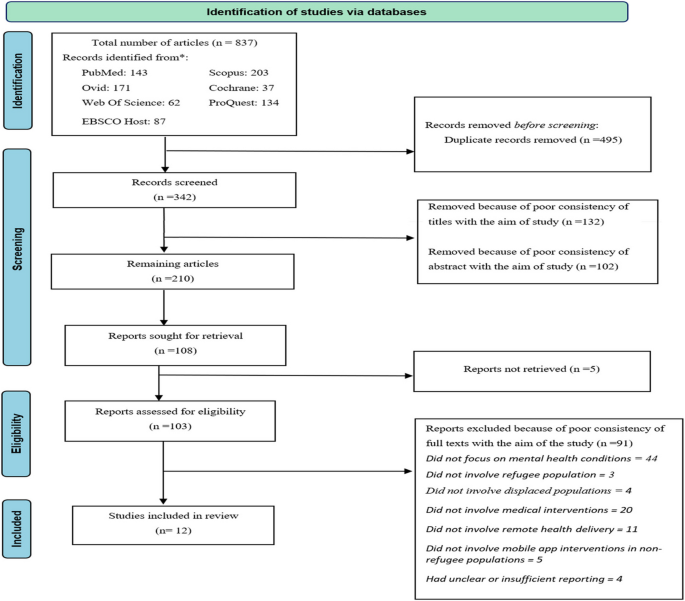
Among these, five studies were not available, so 103 studies were fully and accurately examined. According to the inclusion criteria, 91 studies were excluded and finally, 12 articles were recognized as eligible articles. Full details of the final articles are given in (Table 1).
Demographic and geographic distribution
The reviewed articles encompass a diverse range of refugee populations, including Syrian [38, 42], Afghan [37], Palestinian [37], Central America and the Caribbean [41], Somali-Bantu [44], Nepalese-Bhutanese [44], and Ugandan individuals [44]. While some studies focused exclusively on a single national or ethnic group, others explored broader refugee demographics, capturing a wide spectrum of experiences. The studies were conducted in various geographical contexts, spanning low- to middle-income countries such as Uganda and Turkey, and high-income countries such as Canada and Germany. This geographical diversity highlights the distinct challenges and opportunities in telemedicine for refugee mental health across different socioeconomic settings.
The present research investigates 12 articles published between 2012 and 2023. Geographically, the largest numbers of studies (five) were conducted in Canada, followed by two in the United States, and one each in Turkey, Palestine, Germany, USA, and Uganda. These studies provide a comprehensive view of refugee experiences in different parts of the world.
Regarding research methods, eight of the studies (67%) employed quantitative approaches [37, 38, 40, 42,43,44, 46, 47], while two (17%) used qualitative methods [41, 48], and another two (17%) adopted a mixed-methods approach [39, 45]. This methodological distribution underscores the varied ways researchers have explored refugee experiences and mental health issues.
By examining refugee experiences across different nationalities and geographies and analyzing the diversity of research methods, the present study offers valuable insights and opportunities for deeper analysis of the existing findings. (Fig. 2).
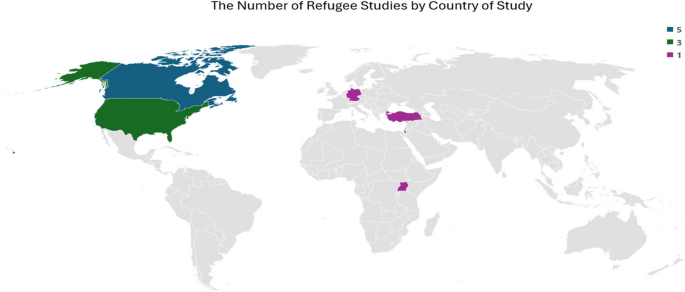
The number of refugee studies by country of study
-Telemedicine interventions
The world of technology and health services is always changing and evolving, and new and modern methods of telemedicine for medical services are constantly being created. This section includes studies that explore telemedicine in mental health interventions, categorized into Virtual Reality, Screening, Investigating Effectiveness, Socio-economic-Cultural Use, Types of Participants, and Using Telemedicine. In mental health interventions, telemedicine has provided a wide range and several studies [37,38,39,40, 42,43,44, 47] have emphasized on the importance of using health along with telemedicine in mental health. In these studies, various software and systems such as CaPRA, Sanadak [42], computer-assisted psychosocial risk assessment software [37], NESTT [44], and web-based mobile health platforms has been used to provide mental health interventions to patients. These software and systems allow mental health service providers to effectively communicate with their patients, collect relevant data, and provide personalized interventions. Therefore, nowadays m-health plays a very significant role in mental health telemedicine. On the other hand, some studies [41, 43, 45, 48] have investigated the effectiveness of intervention methods such as text, video and audio messages. In these studies, platforms such as Google Meet, WhatsApp, Microsoft Teams, FaceTime and other messaging software have been used to provide therapeutic interventions to patients. These methods can be useful as complementary or alternative methods to mhealth-based interventions, especially for patients who do not have access to these technologies or are unwilling to use them. It is important to notice that there is a great diversity in telemedicine intervention methods for mental health. Therefore, the right method for each patient may be different depending on the needs, preferences and individual conditions. Choosing the optimal method for each patient requires accurate evaluation and consideration of various factors such as the severity of symptoms, the level of access to technology, and the patient’s willingness to use technological methods.
Virtual reality
This subsection includes studies on the feasibility, evaluation, and effectiveness of virtual reality (VR) interventions in mental health, focusing on refugee populations [39, 42, 45, 46, 48]. Some studies [42, 46, 48] have dealt with the feasibility, evaluation and effectiveness of computer simulation in mental health. The findings of these articles show the willingness and satisfaction of the participants to use these methods. In one research [45], the integration of virtual care in mental health services for immigrants was used. The results of this study emphasize the potential of this method to facilitate access and remove transportation barriers.
VR refers to 3D computer simulations that people can interact with in real or physical form using certain electronic equipment. This emerging technology is currently receiving attention in various fields including entertainment, education and recently in the field of mental health. Two studies [39, 46] found VR to be effective in reducing mental health symptoms and increasing patient satisfaction. The above researches has shown that using VR could increase patients’satisfaction with the treatment process. Therefore, VR can be used as a tool to provide mental health services to people who do not have access to traditional services, such as people living in rural areas or people with physical disabilities. VR has helped to remove transportation barriers for mental health service recipients, especially for disabled patients who have difficulty getting to a doctor’s office or clinic. VR can provide safe and controlled environments for patients to face their challenges and anxieties in a non-threatening virtual environment. Moreover, the use of VR can increase the motivation of patients to continue treatment while making treatment methods more attractive and interactive.
Screening
Studies in this subsection focus on tools and methods for mental health screening among refugees and vulnerable populations, including HADStress and iCCAS [38, 39]. Considering that the treatment of mental illnesses is a very complex and time-consuming process. One of the important areas that has been mentioned in the studies is screening methods. Screening refers to the initial evaluation of people according to risk factors and risk factors before the appearance of symptoms and disease. In a study [39] that assesses mental health from the perspective of patients and therapists in a community health center, an innovative university-community screening tool iCCAS in English and Spanish has been designed and evaluated. This tool assessed scales such as post-traumatic stress, social determinants of mental health (such as housing, employment status), depression, pervasive anxiety. The results of this study indicated the usefulness, user-friendliness, ease of use, and non-invasiveness of this tool for mental health assessment. While this tool has not been validated for issues such as interaction with providers (monolinguality and the need for a translator), privacy, optimal conditions for screening.
In another study [38], the use of the HADStress screening tool to evaluate four physical factors in mental health, including sleep problems, appetite changes, dizziness and headaches, was investigated. In this tool, the range of scores from zero to four was used to evaluate the variables. According to the questions of this tool, which have a less”threatening”nature compared to other tools such as the trauma screening questionnaire or the PTSD primary care page, the HADStress tool was accepted and satisfied by the participants and nearly half of the participants (45%) showed more willingness to use remote psychiatry; but bilingual women and individuals with a positive stress level (HADS) showed a lower preference for telepsychiatry. However, the rate of relative acceptability of telepsychiatry in Syrian refugees was reported to be good.
Investigate effectiveness
This subsection includes studies evaluating the effectiveness of telemedicine tools such as Sanadak, WelTel, and NESTT, as well as mobile and virtual interventions [42, 44, 46]. In this section, various interventions are evaluated along with the advantages and limitations of telemedicine tools in mental health in articles. Due to the emerging nature of telemedicine in mental health, these studies have investigated different areas of evaluation, efficiency and methods of upgrade, and optimal use of telemedicine in psychiatry. In a study [46], the effectiveness of two mental health interventions among refugee youth (16–23 years old) has been studied using intervention tools, VR scenarios, text messages, and WelTel system on the mobile phone platform to manage messages. In this study, the state of depression, the level of awareness of mental health, the attitude of people regarding seeking help, adaptive coping strategies, the stigma of mental health, and the performance level of refugees have been investigated. The results of the mentioned study showed that by using new and low-cost mental health methods, every patient can easily access health information and required strategies, and mHealth tools lead to easier access of patients to information resources. Moreover, the aforementioned study focused on identifying effective intervention approaches and evaluating evidence-based approaches (such as virtual reality) in different age groups of refugees.
Another study [42] was evaluated the effectiveness and cost-effectiveness of the application (Sanadak) in refugees suffering from post-traumatic stress. The results of this study, according to the CONSORT statement and numerous questionnaires, showed that there is no relationship between the frequency of using the software, education, age groups, gender, and the severity of post-traumatic stress symptoms with the reduction of self-stigma. Sanadak was not effective in reducing mild accident post-traumatic stress, however, it showed a significant reduction in stigma. Also, it was not cost-effective based on the average total adjustment costs and per QALY. However, it was reported cost-effective in the analysis of the causes and motivation of the treatment. Based on the findings of this study, Sanadak is considered an auxiliary and useful tool for post-traumatic stress.
In a study [44], the assessment and control of injustice in mental health services was addressed based on a traumatic stress intervention using a language-free application (NESTT). The findings of the mentioned study showed that after completing the NESTT intervention, the life value scores did not change, however, the participants had a significant reduction in overall psychosocial distress (symptoms related to traumatic stress, anxiety, depression, and physical complaints) And it has shown a reduction in trauma-related symptomology. Moreover, their coping skills and functioning had increased. The findings of this review support the point that using mHealth application will improve mental health outcomes in refugees resettled in the United States. By measuring the effectiveness and feasibility of new and low-cost mental health technology, these studies have the necessary potential for policy, informing and research and application in health, education and social development sectors.
Socio-economic-cultural use
This subsection discusses socio-economic and cultural factors influencing the participation, accessibility, and effectiveness of telemedicine interventions for refugees, drawing from studies on tools like NESTT and culturally adapted programs [37, 39, 44, 45, 47].
Socio-economic and cultural factors significantly influence refugees’willingness to adopt telemedicine, impacting their access to technology, trust in healthcare systems, and communication preferences. Understanding these barriers is key to improving the effectiveness and accessibility of telemedicine interventions for refugee populations. A study by Ahmad et al. [37] explored the psychosocial risks of refugees, particularly focusing on language barriers and socio-economic issues like food insecurity and immigration status. The study found a high willingness (69.6%) among participants to seek psychosocial counseling, emphasizing the importance of culturally adapted tools in facilitating participation. Telemedicine was perceived as reducing social stigma, with patients expressing themselves more openly due to the privacy and accessibility it offered.
While telemedicine offers increased access, several barriers to its utilization persist, particularly in socio-economically disadvantaged groups. Jefee-Bahloul et al. [38] identified key challenges such as language barriers, low literacy levels, and the discomfort some female clients felt when working with male translators. Additionally, socio-economic factors such as financial instability and housing issues were found to impact refugees’mental health, further hindering their access to remote care. These barriers were also observed in a study by Hynie et al. [23], which showed that refugees in deprived areas were less likely to benefit from virtual care compared to those in less deprived neighborhoods, highlighting how socio-economic status and geographic location significantly influence telemedicine use.
Cultural adaptation is crucial for the effectiveness of telemedicine interventions. The NESTT app [44], which used culturally valid visual cues instead of text, was specifically designed with input from cultural experts to accommodate Somali-Bantu and Nepali-Bhutan norms. This adaptation improved the program’s acceptance and engagement, demonstrating the importance of culturally relevant content. Furthermore, Ben-Zeev et al. [40] found that cultural and socio-economic factors such as financial income, family dynamics, and social isolation directly impacted mental health and the effectiveness of virtual care. Financial instability, stigma, and reduced access to social services were among the barriers refugees faced, indicating that addressing these factors is essential to improving intervention outcomes.
Telemedicine can potentially reduce health inequalities by increasing timely access to care for refugee populations. However, socio-economic and cultural issues must be considered to maximize its effectiveness. The use of culturally tailored interventions, like the Sanadak app and the iCCAS tool, has demonstrated potential in engaging marginalized refugee populations. These tools have shown that addressing cultural, linguistic, and socio-economic barriers can improve both patient engagement and satisfaction with care. Additionally, improving access to technology and reducing digital literacy gaps are vital for expanding the reach and effectiveness of telemedicine services.
Types of participants
In refugee health studies, categorizing participants based on their role and expertise provides valuable insights into the perspectives and experiences related to the topic under study. This category generally includes three main groups. Refugees are individuals who have fled their home country due to persecution, war or other dangerous conditions and are currently granted asylum in another country. In the researches [37, 38, 40,41,42, 44, 46], the feasibility and evaluation of mental health interventions were done exclusively on refugees. These studies focused on the direct experiences and mental health needs of refugees.
Health professionals include doctors, nurses, psychologists, social workers and other experts in the field, are crucial in providing mental health services to refugees. In the studies [39, 43, 45, 47], the participating population included health professionals. These studies investigated professionals’perspectives and experiences of mental health services providers to refugees.
In some studies, both groups of refugees and health professionals were used as participants. Research by Hynie et al. [23] participants included refugees and health care workers. This study sought to gain a deeper understanding of the challenges and opportunities associated with providing mental health services to refugees by examining the perspectives of both groups.
Classifying participants by their role and expertise enhances the understanding of study findings, allowing researchers to examine the differences and similarities between groups. The results can then inform the planning and delivery of mental health interventions that cater to the specific needs of each participant group.
Using telemedicine
This subsection explores the methods and challenges of using telemedicine tools, including feasibility, cost, and security considerations [37, 39,40,41,42,43, 45,46,47,48]. In five studies [37,38,39,40, 48] feasibility and investigating the challenges (infrastructure, cost, required technology, privacy and security, behavior and social interaction) and Risk assessment, advantages and disadvantages of remote mental health tools have been discussed, while in other studies [41,42,43,44,45,46,47] investigation the evaluation and effectiveness of telepsychiatry from the point of view of refugees and doctors with The use of different questionnaires, face-to-face and video interviews, telephone, etc. has been discussed.
Also, studies [41,42,43, 45,46,47,48] have shown that telemental health can be effective in the treatment of a wide range of mental disorders, including anxiety, depression, PTSD, substance abuse, and phobias. Remote psychics can be a suitable alternative or complement to face-to-face services for many people. In the studies [37, 40, 42, 44] it has been stated that telehealth is more acceptable for mental health and its evaluation results show the positive opinion of the participants in the studies.
Practical applications
Telemental health has proven to be an effective solution for refugee populations, particularly in overcoming geographical and logistical barriers to mental health care. However, to maximize its impact, it is essential to design these interventions with a deep understanding of the social and cultural contexts of refugee communities. In underserved host countries, the implementation of telemedicine must address systemic barriers related to social justice. Key strategies include ensuring affordable and reliable internet access, empowering community health workers to provide digital literacy training, and creating multilingual platforms that respect local cultural norms and preferences [17, 49, 50]. Studies, such as the use of the NESTT app with Somali-Bantu and Nepalese-Bhutanese refugees, highlight the importance of culturally sensitive tools in fostering engagement and effectiveness [44]. Moreover, interventions like the Sanadak app and virtual reality-based programs should be scaled and adapted to meet the current health, social, and political climates of both refugee populations and their host countries [42].
Evaluating the quality of articles
In this study, the MMAT checklist was used to evaluate the quality and methodology of the articles due to the different types of studies (Supplementary Material 1). In this study, two qualitative studies with an average (6.5 out of 7), three studies of quantitative randomized controlled trials (average 7 out of 7) the highest score, five quantitative descriptive studies (6.2 out of 7) and two mixed methods studies with an average (6.5 out of 7) was used.
Evaluation methods within articles
In the studies, various methods have been used for evaluation; Questionnaire about mental health: according to different issues (depression, PTSD and domestic violence) from different questionnaires in this field in the study [46] of Patient Health Questionnaire- 9, modified depression literacy scale validated in LMICs and Kidcope and CONSORT guidelines, In the study [39] of the ICCAS survey, in [38] the trauma screening questionnaire or PTSD primary care page, in [42] the questionnaire (PHQ- 9, GAD- 7, PHQ- 15, GSE, SSMIS-SF, SMIS -AW SMIS-AG SMIS-AP, SSMIS-HS, RS- 13, LSNS- 6, ENRICHD, Social Support Inventory, EQ- 5D- 5, EQ-VAS, PGI, EuroQoL 5-Dimension 5), in [44] from Valuable Life Questionnaire (VLQ) was used. In studies [37, 39, 42, 44], the usability of the used software was evaluated with different questionnaires, and in all studies the level of satisfaction with it was reported as”acceptable”.
Post-pandemic context
Although most of the studies reviewed were conducted during the COVID- 19 pandemic [37,38,39, 41], we recognize that the overall situation has evolved. The pandemic accelerated the adoption of telemental health, demonstrating its potential to improve access to mental health services for refugees [40, 42]. However, the dynamics of telehealth utilization in the post-pandemic era may differ. This new landscape presents both challenges and opportunities, including variations in resource availability, changes in refugee settlement patterns, and the need to adapt telemental health services to meet the evolving needs of refugee populations [43, 44].
In the post-COVID era, telemedicine faces significant challenges that demand urgent attention to ensure its sustainable integration into healthcare systems. Key issues include strengthening data security to protect sensitive patient information, establishing robust reimbursement policies to incentivize telemedicine adoption, and addressing disparities in internet access to ensure equitable availability of digital healthcare services. These challenges must be prioritized to expand telemedicine’s reach and effectiveness in addressing healthcare needs [51,52,53,54].
The findings of this review, largely derived from the COVID- 19 pandemic [46, 47], lay the groundwork for telemedicine in crisis settings. Yet, post-pandemic scenarios require an adaptation of these solutions to address persistent challenges in refugee mental health care [48]. For example, ensuring stable funding for telemedicine infrastructure, bridging the digital divide, and developing policies for cross-border healthcare delivery are essential steps. The lessons learned from pandemic-driven telemedicine offer valuable insights for shaping long-term strategies to ensure equitable mental health care in refugee contexts [45].


