Global trends
Globally, the number of people aged ≥ 15 years with AUD prevalence increased by 130% between 1990 and 2021, from 84.55 to 111.12 million. However, the age-standardised AUD prevalence decreased from 1,697.90 to 1,335.43 per 100,000 population, with an average annual percent of -0.78% (Table 1). In addition, the number of deaths from AUD also, although rising 158.47 thousand from 110.75 thousand in 1990, the age-standardised AUD mortality decreased from 2.47 to 1.84 per 100,000 population, with an average annual trend of -0.82% (see Supplementary Table S1). Similarly, DALYs from AUD show a similar development, in terms of numbers, from 12.99 million in 1990 to 16.98 million in 2021. But for the age-standardised rate, DALYs from AUD decreased from 266.11 per 100,000 to 202.39, with an average annual trend of -0.83% (see Supplementary Table S2). The declines in age-standardised AUD prevalence, mortality, and DALYs suggest that the global burden of AUD is on a declining trend.
Global trends by sex
From 1990 to 2021, the global prevalence of AUD among people aged ≥ 15 years increased (males: from 65.24 million to 86.20 million; females: from 19.31 million to 24.92 million), but the age-standardised AUD prevalence declined (males: from 2,168.80 to 2,077.27 per 100,000; females from 744.59 to 599.50). The decline in AUD was slightly larger in females (-0.82%Vs-0.75%) over the same period (see Table 1). Further, our results from ARIMA model projections indicated that in 2040, the age-standardised prevalence of AUD is projected to be 1782.33 per 100,000 for males and 452.23 per 100,000 for females (see Supplementary Figure S1). In addition, AUD-related age-standardised mortality and age-standardised DALYs declined between 1990 and 2021 for both males and females, with the decline being more pronounced for females than for males (AUD age-standardised mortality: -1.22%Vs-0.73%; AUD age-standardised DALYs: -0.95%Vs-0.79%) (see Supplementary Figure S2 and Supplementary Tables S1 and S2). These findings suggest that males are likely to remain the primary group affected by AUD globally, both currently and in the future.
In addition, age-standardised AUD prevalence, mortality and DALYs were higher for males than for females, irrespective of changes in sociodemographic indices (see Supplementary Fig. 4). However, the results were more complex for AAPCs. Globally, for AUD prevalence, mortality, and DALYs for AAPCs, the decline was more pronounced for females than for males (see Supplementary Figure S5). However, in high SDI regions (males: -0.55%; females: -0.17%), middle SDI regions (males: -0.52%; females: -0.45%), low-middle SDI regions (males: -0.82%; females: -0.33%), and low SDI regions (males: -0.47%; females: -0.32%), the age-standardised prevalence of AUD declined more significantly among males than females. Regarding AUD-related age-standardised mortality, there was an upward trend for females in high SDI regions (0.55%), in contrast to a downward trend for males (-0.19%). For AUD-related age-standardised DALYs, the decline was consistently smaller for females than for males in high SDI regions (males: -0.50%; females: -0.01%), low-middle SDI regions (males: -0.72%; females: -0.47%), and low SDI regions (males: -0.47%; females: -0.44%). This evidence suggests that although the current state of AUD burden may be smaller for females than for males, this difference in AUD burden between males and females is diminishing in specific areas (e.g., high SDI areas) because the decline in AUD among males is occurring at a faster rate than that among females.
Global trends by age subgroup
Previous studies have rarely considered the status and trends of AUD in different age groups [2]. The results show that globally, people younger than 55 years of age have higher AUD-related prevalence, mortality and DALYs compared to older people after 55 years of age, but as the decline in this indicator is larger for people younger than 55 years of age, this suggests that the gap is narrowing(see Table 1, Supplementary Table S1 and Supplementary Table S2). Specifically, all age groups except the 70–74 age group showed decreasing trends in AUD prevalence, with the largest decreases of more than 1% in young adults aged 20–29 years (see Table 1). Furthermore, as the AAPCs were not statistically significant (p >.05), this implies that AUD mortality did not decline significantly in the 55–59, 60–64, 65–69, and 70–74 age groups (see Supplementary Table S1). For AUD DALYs, a decreasing trend was observed in all age groups except the 70–74 age group (see Supplementary Table S2). This evidence suggests that attention needs to be paid to the burden of AUD in relative older (e.g., 55 + years) adults.
Furthermore, we found that globally, the burden of AUD, as measured by prevalence, mortality and DALYs, declined significantly across all age subgroups, except for women 55–59 years, for whom the decline in AUD mortality was not statistically significant (p =.094) (see Supplementary Table S3). In contrast, older male adults did not show a significant trend of decreasing risk. Specifically, there was no significant decline in the prevalence of AUD in men aged 70 years or older; nor was there a significant decline in AUD mortality in males aged 55–74 years, nor in AUD DALYs in males aged 65–74 years (see Supplementary Table S3). Further, we found that in high SDI regions, adults aged 60 + were at risk of rising AUD-related prevalence, mortality, and DALYs, while adults aged 55–59 + years were also at risk of rising AUD mortality and DALYs. In addition, in the middle SDI, older adults aged 70 + faced rising AUD prevalence (see Supplementary Table S4 and Supplementary Figure S6). The results suggest that older populations (e.g., those aged over 55 years) may be facing an increasingly higher burden of alcohol use disorders.
Global trends by sociodemographic index
Globally, age-standardised prevalence due to AUD is declining significantly in all regions over the period 1990–2021, particularly in high-middle SDI regions, with an AAPC = -0.92%, and in high SDI regions, to a lesser extent, with an AAPC of -0.41% (see Table 1). In terms of age-standardised mortality due to AUDs, all regions showed a significant decline, except for high SDI regions (AAPC = 0.02%; see Supplementary Table S1). AUD-related age-standardised DALYs declined in all regions, particularly in the high-middle SDI regions, where the AAPC = -1.11%, compared with a smaller decline in the high SDI regions, where the AAPC = -0.34% (see Supplementary Table S2). Although high-middle SDI regions had higher AUD-related age-standardised prevalence, mortality and DALYs in 1990, high SDI regions already had the highest AUD-related age-standardised prevalence (1,847 per 100,000), mortality (2.58 per 100,000) and DALYs (278.84 per 100,000) in 2021, due to the slower decline in high SDI regions.
Regional trends
From 1990 to 2021, Australasia and Oceania demonstrated an increase in the age-standardised prevalence of AUD, with AAPCs of 0.6% and 0.12%, respectively. With the exception of East Asia (AAPC=-0.19, p =.168), all regions significantly showed a significant decrease in the age-standardised prevalence of AUD (see Supplementary Table S5).
From 1990 to 2021, Caribbean (AAPC = 0.11%), East Asia (AAPC = 0.22%), and High-income North America (AAPC = 1.28%) demonstrated an upward trend in AUD-related age-standardised mortality. Moreover, no significant changes were observed in the AUD-related age-standardised mortality rates for Australasia (AAPC = 0.11%, p =.824), Central Europe (AAPC = -0.22%, p =.678), and Eastern Europe (AAPC = -0.19%, p =.813). Further, the rest of the regions showed significant decreases in age-standardised mortality for AUD (see Supplementary Table S6).
From 1990 to 2021, Australasia (AAPC = 0.42%, p <.001) showed a significant increase in age-standardised DALYs dut to AUD. In contrast, the Caribbean (AAPC=-0.08%, p =.613), Central Europe (AAPC=-0.39%, p =.089), East Asia (AAPC=-0.12%, p =.167), Eastern Europe (AAPC=-0.41%, p =.394), and High-income North America (AAPC=-0.04%, p =.627) did not exhibit statistically significant changes in AUD-related age-standardised DALYs. All other regions showed significant declines in AUD-related age-standardised DALYs (see Supplementary Table S7).
In addition, after stratifying by sex, Eastern Europe males had the highest age-standardised prevalence, mortality and DALYs due to AUD in 2021. Similarly, Eastern Europe females had the highest AUD-related age-standardised prevalence, mortality and DALYs (see Supplementary Table S8).
National trends
At the national level, from 1990 to 2021, Mongolia, United Kingdom, and New Zealand had the highest age-standardised AUD prevalence increases of 2.04%, 1.12%, and 1.06%, respectively. Furthermore, Cuba, United Kingdom, and Paraguay had the highest increases in age-standardised AUD mortality of 2.78%, 2.42%, and 1.97%, respectively. Finally, Mongolia, the United Kingdom, and New Zealand witnessed the highest age-standardised AUD DALYs increases, at 1.79%, 1.22%, and 0.92%, respectively (see Figs. 1 and 2, and 3; see Supplementary Table S9).
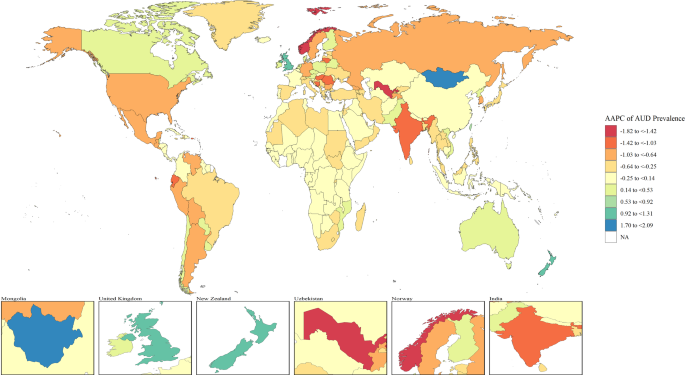
Map showing average annual percentage change in global prevalence of alcohol use disorders in adults, 1990–2021. Note: AAPCs = average annual percent changes; AUD = alcohol use disorders
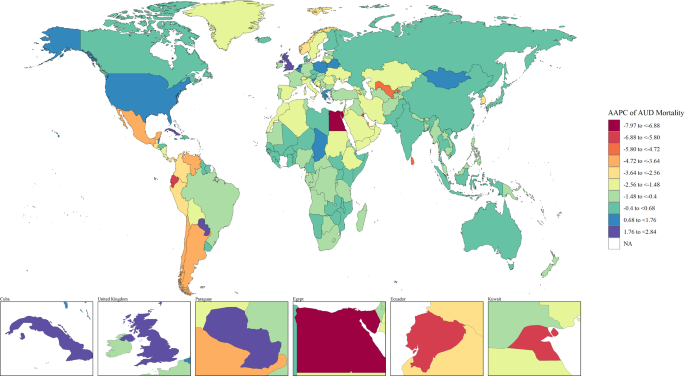
Map showing average annual percentage change in global mortality of alcohol use disorders in adults, 1990–2021. Note: AAPCs = average annual percent changes; AUD = alcohol use disorders
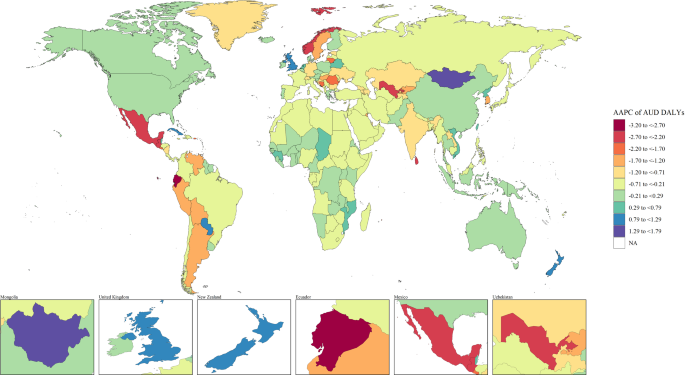
Map showing average annual percentage change in global disability adjusted life years of alcohol use disorders in adults, 1990–2021. Note: AAPCs = average annual percent changes; AUD = alcohol use disorders; DALYs = disability adjusted life years
Risk factors
Detailed analyses of global data from 1990 to 2021 show that the two main risk factors associated with AUD among people ≥ 15 years of age are high alcohol use and childhood sexual abuse (Table 2). In 2021, globally, the age-standardised DALYs from high alcohol use were 202 per 100,000 people and 15.83 per 100,000 for childhood sexual abuse. In addition, from 1990 to 2021, these factors correspond to an AAPC of -0.83% and − 0.87%, respectively.
High alcohol use DALYs declined fastest in high-middle SDI regions (AAPC = -1.11%) and slowest in high SDI regions (AAPC = -0.34%). Similarly, childhood sexual abuse DALYs declined most rapidly in high-middle SDI regions (AAPC = -1.48%) and most slowly in high SDI regions (AAPC = -0.04%).


